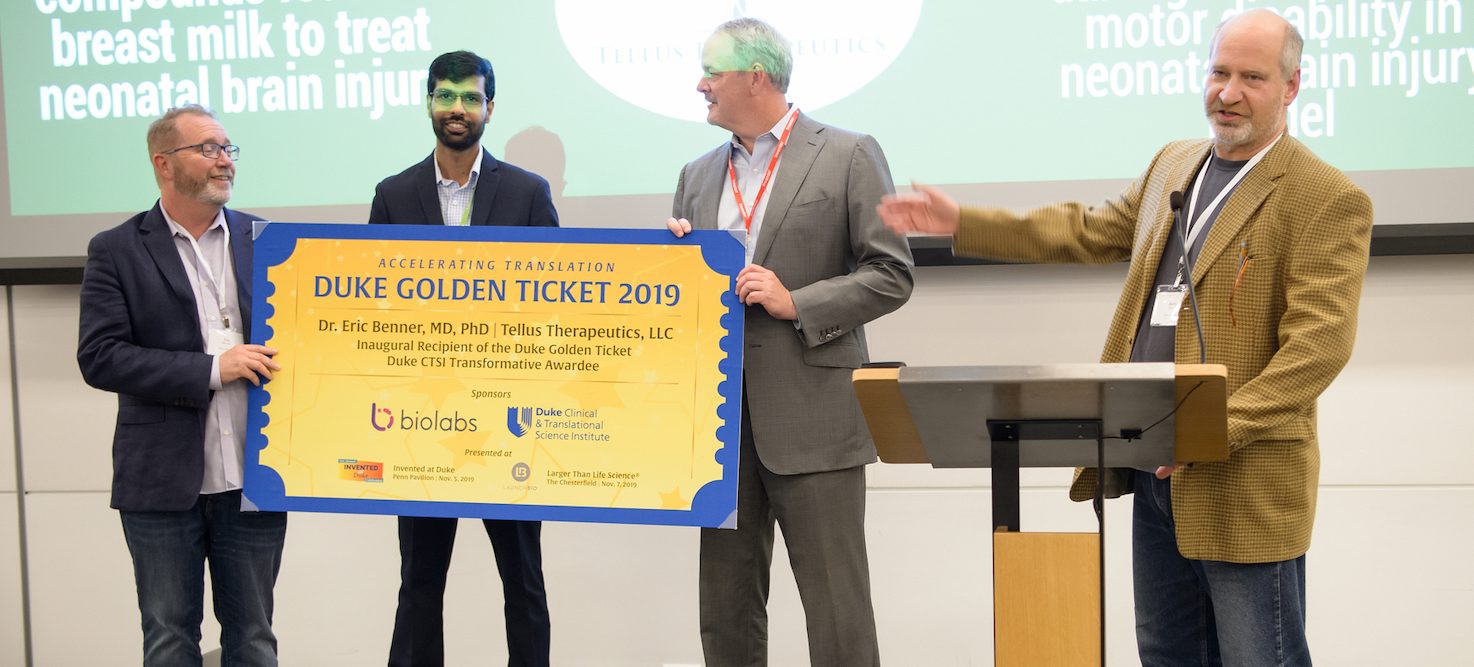
(Durham, NC and New York, NY, December 18, 2019)—Duke University and Deerfield Management Company, a healthcare investment firm, today announced the creation of a major translational research collaboration. Spearheaded by Duke University’s Office of Licensing & Ventures (OLV), the alliance is expected to accelerate the preclinical development of new drugs for improved quality of life and cures for disease.

“This is an exciting day for Duke and the patients we serve,” said Mary E. Klotman, MD, Dean, Duke University School of Medicine and Vice Chancellor for Health Affairs. “This new partnership will help further Duke’s commitment to improving the lives of people in our own community and around the world by supporting and accelerating the translation of research into new therapies to treat and cure society’s most formidable healthcare challenges.”
By way of a newly launched company called Four Points Innovation, up to $130 million of initial funding will be made available by Deerfield to back the initiative for 10 years. Deerfield also will provide development expertise in support of Duke’s innovative drug research across a span of high-need therapeutic areas, as well as those targeting patients who suffer from hard-to-treat and rare diseases.
A private company wholly owned by affiliates of Deerfield, Four Points Innovation will support Duke R&D projects throughout preclinical stages of drug discovery and development. Beginning approximately in March 2020, Duke researchers will have the ability to submit proposals on projects for consideration by a Four Points Innovation committee comprised of scientific leadership representing both Duke and Deerfield.
Accepted projects will include a development plan aimed at achieving Investigational New Drug (IND) readiness. Deerfield will provide funding and operational support for accepted projects, and successful projects that achieve IND-enabled status may be eligible for additional capital from Deerfield.
Duke’s Office of Licensing and Ventures broke previous records last year with 354 invention disclosures, 120 agreements, and 32 exclusive agreements. Duke faculty and staff formed sixteen new start-up companies during the year, bringing the university’s total to over 140 new companies. Over the last two years, 29 of the university’s 32 startups have chosen to stay in North Carolina.
“Duke University, with its vast research enterprise, world-class investigators and novel innovations, is a leader in biomedical discovery,” said James E. Flynn, Managing Partner at Deerfield Management. “We are excited about entering into this partnership with Duke, as we collectively seek to develop new medicines to save lives and address unmet medical needs.”
Under the terms of the agreement, Four Points Innovation would receive an option to license Four Points Innovation-funded intellectual property developed at Duke.





 Although there is a long history of research into engineering disease-resistant plants, a practical application for using these methods in crops results in lower crop yield as the plant is diverting its energy to maintaining a constant active defense.
Although there is a long history of research into engineering disease-resistant plants, a practical application for using these methods in crops results in lower crop yield as the plant is diverting its energy to maintaining a constant active defense.





 Inventor: Xinnian Dong
Inventor: Xinnian Dong Inventors: Bruce Donald, Marcel Frenkel, Mark Hallen, Jonathan Jou
Inventors: Bruce Donald, Marcel Frenkel, Mark Hallen, Jonathan Jou Inventor: Scott Soderling
Inventor: Scott Soderling Inventors: Allen Song, Dean Darnell, Trong-Kha Truong
Inventors: Allen Song, Dean Darnell, Trong-Kha Truong Inventor: Muath Bishawi
Inventor: Muath Bishawi Inventors: Alvin Lebeck, Craig LaBoda, Chris Dwyer
Inventors: Alvin Lebeck, Craig LaBoda, Chris Dwyer Inventors: Kamran Mahmood, Paolo Maccarini, Donald Pearce
Inventors: Kamran Mahmood, Paolo Maccarini, Donald Pearce Inventors: Tracy Futhey, Richard Biever
Inventors: Tracy Futhey, Richard Biever Inventor: Ken Gall
Inventor: Ken Gall Inventor: Michael Klien
Inventor: Michael Klien Inventors: Kevin Gehsmann, Clark Bulleit, Tim Skapek
Inventors: Kevin Gehsmann, Clark Bulleit, Tim Skapek Inventor: Beryl Baldwin
Inventor: Beryl Baldwin Inventor: Erikson Nichols
Inventor: Erikson Nichols








